A 42-year-old woman comes to the emergency department due to shortness of breath. Approximately 2 weeks ago, the patient developed shortness of breath on exertion that has become progressively worse. She also reports mild chest pain with deep inspiration. She has had no weight loss, fever, cough, or sputum production. Medical history includes diet-controlled type 2 diabetes mellitus and locally advanced infiltrating ductal carcinoma of the left breast, for which she underwent neoadjuvant chemotherapy followed by surgical resection and radiation approximately 2 years ago. The patient is a lifetime nonsmoker and has no significant second-hand tobacco exposure. She lives with her family and works as a teacher. Family history is notable for colon cancer in her father.
Temperature is 37.6 C (99.7 F) , blood pressure is 122/78 mm Hg, pulse is 92/min, and respirations are 20/min. Oxygen saturation is 92% on ambient air. Physical examination shows moist mucous membranes with no jugular venous distension or lymphadenopathy. Heart rate is regular with no murmurs or gallops. Auscultation reveals decreased breath sounds over the right lower lung with dullness to percussion. Extremities have no edema. The remainder of the examination is normal. Upright chest x-ray reveals the following: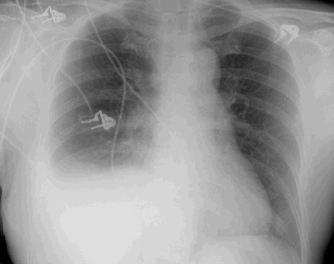
The patient undergoes thoracentesis. Pleural fluid analysis shows 3,500/mm3 nucleated cells, predominantly lymphocytes. Additional pleural fluid analysis results are as follows: Gram stain and culture of the pleural fluid are negative. What is the most appropriate next step in management of this patient?
Gram stain and culture of the pleural fluid are negative. What is the most appropriate next step in management of this patient?
Definitions:
Norepinephrine
Norepinephrine is a neurotransmitter and hormone important in the body's fight or flight response, involved in increasing heart rate and blood pressure.
Sympathetic Nerve
Part of the autonomic nervous system that stimulates the body's fight or flight response.
Sympathetic Control
The regulation of bodily functions by the sympathetic nervous system, which activates the body's "fight or flight" response.
Heart
A muscular organ that pumps blood through the circulatory system, supplying oxygen and nutrients to the tissues and removing carbon dioxide and other wastes.
Q2: The heading of an office legal memorandum
Q4: The law component of the issue may
Q12: If times have changed and there is
Q67: The formula <img src="https://d2lvgg3v3hfg70.cloudfront.net/TBX8672/.jpg" alt="The formula
Q85: An 83-year-old man with mild cognitive impairment
Q127: A 40-year-old man comes to the emergency
Q166: A 62-year-old man comes to the office
Q339: A 74-year-old man comes to the physician
Q650: A 54-year-old woman comes to the office
Q850: A 42-year-old man comes to the office