T10-1A OPERATIVE REPORT, LYMPHADENECTOMY
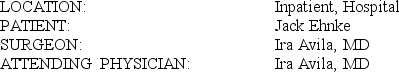 PREOPERATIVE DIAGNOSIS: History of adenocarcinoma of the prostate, with elevated PSA (prostate specific antigen)
PREOPERATIVE DIAGNOSIS: History of adenocarcinoma of the prostate, with elevated PSA (prostate specific antigen)
POSTOPERATIVE DIAGNOSIS: Recurrent adenocarcinoma of the prostate
ANESTHESIA: General
PROCEDURE: Please see the preoperative note for indications of the procedure as well as full informed consent. The patient underwent a general anesthetic and was put in a modified frog-leg position. Anesthesia preparation included a central venous line, arterial line, and epidural catheter. After this was achieved, a midline incision was made between the umbilicus and symphysis pubis. This was deepened down through skin and generous subcutaneous tissue to the midline. The retropubic space was entered and developed. The pelvic lymphadenectomy was then performed. This was carried along the usual lines. The lateral extension was the external iliac vein. Tissues surrounding that vein were brought down and around the muscle wall to include the obturator group, preventing injury to the obturator artery, vein, and nerve. Proximally we went to the circumflex iliac branches, including the node of Cloquet, and then used clips across the trunks of the lymphatics. Distally or proximally on the patient, we proceeded to the bifurcation of the iliac vein, ending the dissection at that point. Again, the lymphatic trunks were clipped. Each package was delivered and sent to Pathology for frozen section analysis. With the result of negative nodes, we proceeded with surgical removal of the prostate. This was performed in standard fashion. The Thompson retractor was used with modifications under padded retractors throughout the procedure. This allowed adequate exposure. The margin between the lateral and endopelvic fascia was opened in anteromedial fashion to the puboprostatic ligaments, which were opened. The patient's size was fairly good, and he had a large prostate so the visualization in the apical area of the prostate was not so great. We finger dissected along the superficial venous complex, reaching the apex of the prostate on each side. The McDougall clamp was placed through the fascia under the superficial venous complex but anterior to the urethra. Space was created there. A TIA-46 stapler was used to staple across the superficial venous complex. The urethra was exposed and opened anteriorly. Sutures at 10 and 2 o'clock were placed, 2-0 chromic, outside to in. The rest of the urethra was mobilized after the catheter was brought up and out of the wound and used for traction device after it was cut. The urethra was incised, and sutures were placed at the 4 and 8 o'clock positions likewise. Apex of the prostate was mobilized using sharp and blunt dissection, carrying it down to the lateral pelvic fascial leaves. These were separated using sharp and blunt dissection off the lateral aspect of the prostate. Clips were used for the small bleeding vessels encountered. The lateral pedicle was then mobilized between clamps and ligated with 0 chromics, each side. Care was again taken to avoid the neurovascular bundle apparatus. The prostate was mobilized anteriorly, and the Denonvilliers' fascia was opened over the seminal vesicles. Those were dissected posteriorly. The bladder neck was then incised down just behind the prostate. Because of the large median lobe on the prostate, we had to open the bladder neck somewhat more than normal. We exposed the trigone but did not approach it. The prostate was dissected posteriorly off the bladder neck using sharp and blunt dissection. The seminal vesicles were then approached anteriorly, as was the ampulla of the vas. Each was cross-clamped and ligated. Final hemostasis was achieved at this point with the prostate removed. We everted the urothelium and closed the bladder neck slightly. We then brought the sutures concomitantly from inside to out, at 2, 10, 4, and 8 o'clock. An 18-silicone catheter was placed in the bladder, and the sutures were tied down. Hemovac drains were placed, and the wound was closed with a double-stranded running nylon. Skin clips were placed, and the drains were secured. He tolerated the procedure well overall.
PATHOLOGY REPORT LATER INDICATED: Adenocarcinoma neoplasm, prostate, benign lymph nodes
T10-1A:
SERVICE CODE(S): ___________________________________________________
ICD-10-CM DX CODE(S): ______________________________________________
Definitions:
Hallucinations
Experience of sensing things while awake that appear to be real but instead have been created by the mind.
Sensations
Feelings or perceptions resulting from something that happens to or comes into contact with the body.
SAD
Seasonal Affective Disorder, a type of depression that occurs at a particular time of the year, usually in winter.
Altered Consciousness
Any state of awareness that is significantly different from the normal waking state, including states of heightened awareness or conditions like coma.
Q1: T6-2C PROGRESS NOTE<br> <img src="https://d2lvgg3v3hfg70.cloudfront.net/TB6048/.jpg" alt="T6-2C PROGRESS
Q6: AUDIT REPORT T8.1 OPERATIVE REPORT, CLOSED REDUCTION<br>
Q7: T10-2C TRANSRECTAL ULTRASOUND<br> <img src="https://d2lvgg3v3hfg70.cloudfront.net/TB6048/.jpg" alt="T10-2C TRANSRECTAL
Q21: Kouba Manufacturing Corporation's actual direct labor
Q36: The debits to the Raw Materials account
Q42: The management of Harrigill Corporation would like
Q46: Lacy Corporation uses the absorption costing approach
Q58: The markup on absorption cost is closest
Q62: Joeston Corporation makes a product with
Q101: Which of the following statements regarding fixed