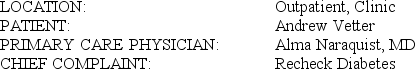
AUDIT REPORT T1.1 OFFICE VISIT
 He has started doing PT to get his strength back and has noted improvement. He has not been having any chest pain or SOB. Past history of CAD.
He has started doing PT to get his strength back and has noted improvement. He has not been having any chest pain or SOB. Past history of CAD.
His DM has been variably controlled. He is taking Lantus 28 units in the evening and Humalog 12 units with meals. He is testing 2-4 times per day. He is having reactions around 3 PM about once a week. He does get a warning with the reactions. His sugars are highly variable at all testing times with high and low sugars. His evening sugars tend to be high, and he may overeat after supper.
He continues to have numbness in the feet. There is no edema. His depression seems to be ok.
EXAM: Vitals:Weight is 180. Blood pressure is 120/70. Patient is alert and conversant.
He is near his ideal weight. There is no edema. The foot pulses are normal. The ankle and knee reflexes are normal. There is a slight decrease in the vibratory sensation. The chest is clear. Cardiac: The heart is regular with no murmur or S3. The abdomen is soft and nontender with no masses. The prostate is a little enlarged with no masses. The rectum is normal, and there are some small hemorrhoids noted. The stool is hemoccult negative.
IMPRESSION: 1) DM Type 1 with variable control, 2) Hemorrhoids, 3) CAD, stable.
PLAN: Anusol suppository bid prn and tub soaks. He may need to cut the noon Humalog by 2 units. See in 4 months with an HgbA1c.
T1.1:
SERVICE CODE(S): 99213_________________________________
ICD-10-CM DX CODE(S): E10.9____________________________
INCORRECT/MISSING CODE(S):__________________________
Definitions:
Sensorimotor Stage
Piaget’s initial major stage of cognitive development, which can be broken down into six substages.
Sociocultural Approach
A theoretical perspective that emphasizes the impact of social and cultural factors on individual behavior and cognitive processes.
Multiple Perspectives
The approach of considering and integrating diverse viewpoints and angles in analysis, problem-solving, or understanding complex issues.
Q3: The manufacturing overhead that would be applied
Q7: The net present value of the project
Q15: The selling and administrative expense adjusted to
Q17: Harkey Corporation's statement of financial position and
Q20: Up to how much should the company
Q21: The Stephens Leadership Center provides training
Q23: The credits to the Raw Materials account
Q33: Assume that after introducing the new product,the
Q38: Perin Corporation would like to use target
Q75: What would be the total variable inspection